Are your eyes sensitive to certain kinds of light? Have you considered how FL-41 lenses, Avulux and blue light glasses could reduce your susceptibility?
Choosing the right type of glasses can significantly improve your quality of life if your eyes react badly to certain light conditions. In this article I want to share with you the differences between three types of eyewear that you should know about.
I’m Juliet Menakaya, the owner and principal optometrist at Junic Eye Care in Canberra. At our clinic, we pride ourselves on our extensive experience in treating patients of all ages suffering from light induced discomfort. Our approach is tailored to each individual, ensuring that every visit addresses your specific eye health needs with understanding and professional care.
Light Sensitivity and Your Eyes
Why do some people find bright lights unbearably uncomfortable while others don’t seem to be bothered at all? Light sensitivity, or photophobia, can be a perplexing and often debilitating issue caused by various underlying conditions.
- Dry eyes can lead to light sensitivity because the lack of adequate moisture on the eye’s surface can make it more prone to irritation from light. This condition often results from prolonged screen time or environmental factors.
- Blepharitis, an inflammation of the eyelids, can also cause sensitivity to light. This condition leads to swollen, irritated eyelids, which can increase the eye’s overall sensitivity.
- Eye infections can increase sensitivity to light as they often involve inflammation and irritation of the eye tissues. Conditions like conjunctivitis can make your eyes more reactive until the infection is resolved.
- Corneal abrasions can cause significant light sensitivity due to the damage they inflict on the eye’s surface. These scratches make the eye more vulnerable to light, causing pain and discomfort.
- Photokeratitis, a condition similar to sunburn of the eye, can cause light sensitivity. This is often a result of excessive exposure to UV light, leading to inflammation and pain in the eyes.
- People with blue eyes have less pigment to protect against harsh lighting conditions. This makes them more susceptible to discomfort in brightly lit environments.
- Migraines are a common cause of light sensitivity, making bright lights intolerable during an episode. This symptom can significantly impact daily activities and quality of life.
- Blepharospasm, an involuntary eyelid twitch, can also lead to light sensitivity. The constant twitching can make the eyes more sensitive to harsh lighting and exacerbate discomfort.
Understanding the root causes of photophobia is essential for effective management. With proper eye care and protective measures you can significantly reduce the impact of light sensitivity on your daily life.
Watch the following video by Dr. Rupa Wong as she explains why light can impact on our level of eye comfort.
The Role of FL-41 Glasses in Managing Light Sensitivity
Developed in the early 1990s, rose-colored tint FL-41 glasses were initially designed to help patients with fluorescent light sensitivity. Over time, their effectiveness has been well documented.
FL-41 glasses work by filtering out specific wavelengths of light which are known to trigger migraines. This targeted approach helps reduce the intensity of bright lights, making it easier for patients to function in various lighting conditions without discomfort.
In tests of FL-41-filtered lenses against conventional gray sunglasses and standard rose-tinted spectacles, researchers found that the majority of patients preferred wearing FL-41-filtered spectacles.
For migraine sufferers, FL-41 glasses can provide substantial relief. Studies have shown that these glasses can decrease both the frequency and severity of migraines, offering a non-pharmacological treatment option. This is particularly beneficial for individuals seeking to avoid medication side effects or looking for additional support in managing their symptoms.
Understanding Avulux Glasses
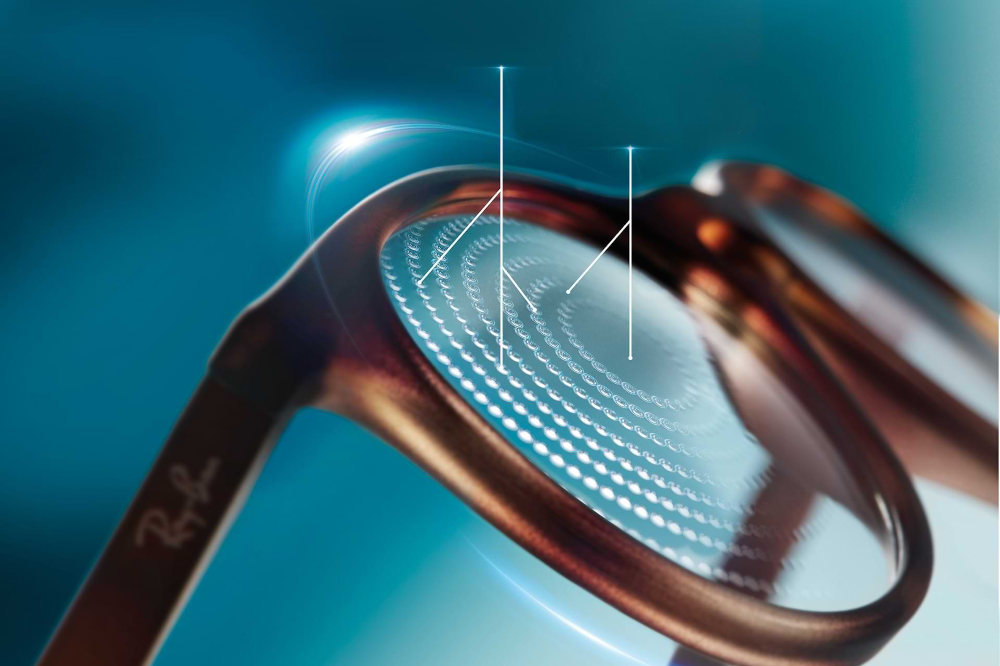
How do Avulux glasses work to alleviate migraines? Similar to FL-41 lenses, Avulux glasses are specifically designed to filter out certain wavelengths of light. By selectively blocking blue, amber, and red light, these glasses create a more comfortable visual environment for sufferers of light sensitivity.
Unlike FL-41, Avulux has the appearance of a neutral, gray tint and does not distort colors. For individuals with photophobia (light sensitivity), Avulux glasses provide more extensive protection against bright outdoor light, which can be overwhelming and trigger migraines or discomfort. The enhanced filtering helps to reduce glare and light intensity more effectively than FL-41 lenses.
Preliminary research conducted at the University of Utah also indicates that Avulux may also help patients with visual snow syndrome, a disorder that causes you to see static. Some describe it as seeing things in a snow globe that’s been shaken up.


Blue Light Glasses Explained
Blue light glasses are designed to filter out the blue light emitted by digital screens, which is a significant contributor to eye strain and light discomfort. These glasses are increasingly popular among people who spend extended periods in front of computers, tablets, and smartphones.
Scientific studies have questioned the effectiveness of blue light glasses in reducing digital eye strain. While some may argue that the evidence is mixed, many users report noticeable improvements in their symptoms when using these glasses. It’s important to note, however, that blue light glasses are not a cure-all; they work best when combined with other eye care practices, such as taking regular breaks and adjusting screen settings.
Comparative Analysis: FL-41, Avulux, and Blue Light Glasses
How do Avulux, FL-41, and blue light glasses compare? Each type offers unique benefits tailored to specific needs. Avulux glasses are particularly effective for migraine sufferers, filtering out a broad spectrum of light wavelengths that trigger headaches. FL-41 glasses, with their focus on blue and green light, are highly specialised for reducing light sensitivity.
On the other hand, blue light glasses are designed primarily to alleviate digital eye strain, making them ideal for those who spend long hours in front of screens. While they provide some relief for headaches, their primary function is to enhance comfort during screen use.
Choosing the right pair depends on your specific symptoms and needs. At Junic Eye Care, we help you find the best solution to improve your daily comfort and eye health.
| Features | Avulux Lenses | Generic FL-41 Lenses (TheraSpecs, Somnilight, etc.) |
Generic Blue Light Glasses or Sunglasses |
|---|---|---|---|
| Precision Tinted Lenses | Multi-Band | Single-Band | ✖ |
| Does Not Distort How You Perceive Color | ✔ | ✖ | Some Brands |
| Filters Up to 90% of Harmful Blue Light | ✔ | Some Brands | ✖ |
| Filters Up to 97% of Harmful Amber & Red light | ✔ | ✖ | ✖ |
| Allows in Over 70% of Soothing Green Light While Filtering Harmful Light | ✔ | ✖ | ✖ |
| Patented | ✔ | ✖ | ✖ |
| Clinically Proven and May Help People with Migraine by Precisely Filtering Light | ✔ | ✖ | ✖ |
| Premium Frames | ✔ | – | – |
| Effective Light Management Indoors or Outdoors With the Same Lenses | ✔ | ✖ | ✖ |
Source: https://avulux.com/pages/migraine-light-sensitivity-photophobia-glasses-comparison
Where to Get Tested and Fitted in Canberra
Where can you get the right eyewear to address your eye strain and migraines? At Junic Eye Care, we offer comprehensive eye exams and fittings tailored to your specific needs. Our experienced optometrists will assess your eye health, discuss your symptoms, and recommend the most suitable eyewear, whether it’s Avulux, FL-41, or blue light glasses.
Booking an appointment with us is straightforward. You can visit our website or call our clinic to schedule a consultation. During your visit, we’ll conduct a thorough examination and provide personalised advice to help you manage your eye health effectively.
CONCLUSION
This article compares Avulux, FL-41, and blue light glasses, focusing on their specific benefits in combating light sensitivity, migraines and digital eye strain in Canberra’s office-heavy workforce.
Without the right glasses, you may continue to suffer from headaches and irritation, impacting your work efficiency and overall quality of life.
Ignoring the need for specialized eyewear can lead to a reliance on temporary solutions, such as over-the-counter pain medication, which doesn’t address the root cause of your discomfort.
Don’t wait for your eye discomfort to worsen; be proactive and schedule a consultation to explore how specialized glasses can transform your daily life.
To visit our optometry practice, click the “Book Online” button at the top of the page or call (02) 6152 8585 today.
You’ll find our clinic conveniently located in the Molonglo Health Hub, just a short 10 minute drive from central Canberra, with plenty of free parking when you get here.

CANBERRA OPTOMETRIST
Juliet obtained her Doctor of Optometry degree from the University of Benin, Nigeria in 2006. She completed an internship programme before migrating to Australia, where she completed a master’s degree in public health at the University of Sydney in 2014. Following this, Juliet obtained a Master of Orthoptics from the University of Technology Sydney (UTS) in 2017.
Juliet has completed her competency in optometry examination with OCANZ (Optometry Council of Australia and New Zealand), and obtained her ophthalmic prescribing rights from ACO (Australian College Of Optometry Victoria). Juliet has worked in various positions, including retail Optometry, the Ophthalmology Department at Canberra Hospital, and more recently, at the John Curtin School of Medical Research (ANU).
As a dedicated Canberra optometrist, Juliet is passionate about helping people with low vision, and binocular vision anomalies hence her interests in Low Vision Rehabilitation, Eccentric Viewing Training and Paediatric optometry.