Discover how to determine eligibility for free cataract surgery in Canberra ACT, focusing on Medicare options and private costs. Navigate surgery expenses with confidence.
Understanding Eligibility for Free Cataract Surgery
Cataract surgery is a crucial procedure for many individuals experiencing vision problems due to cataracts. These cloudy areas in the lens of the eye can significantly impair vision, leading to difficulties in daily life. However, the costs associated with cataract surgery can be a concern for many, especially seniors and pensioners. This guide will help you understand the eligibility for free cataract surgery, particularly in Canberra, and provide insights into the costs involved in private surgeries.
What is Cataract Surgery?
Cataract surgery involves removing the cloudy lens and replacing it with a clear artificial lens. This procedure is typically quick, with a high success rate, allowing patients to regain clear vision. Understanding the financial aspects of this surgery is essential for those who need it is very vital in making decisions on when and where to have your surgery.
Free Cataract Surgery for Seniors in Canberra
For many seniors in Canberra, the cost of cataract surgery is a significant concern. Fortunately, there are programs and government assistance available to help alleviate these costs.
Medicare Coverage
Medicare plays a significant role in covering the cost of cataract surgery for eligible Australians. While Medicare does not cover the entire cost, it significantly reduces the financial burden. The coverage includes a portion of the surgeon’s fee and hospital charges if the procedure is performed in a public hospital.
Who is Eligible?
Eligibility for Medicare-covered cataract surgery primarily depends on the patient’s age, residency status, and specific medical needs. Seniors and pensioners typically have access to these benefits, but it’s essential to check individual eligibility criteria with Medicare.
Bulk-Billed Cataract Surgery
In some cases, cataract surgery can be bulk billed, meaning there are no out-of-pocket expenses for the patient. Bulk-billing is more common in public hospitals and specific clinics, where the costs are covered entirely by Medicare. However, the public hospitals have long waiting lists, potentially 6-18 months or even longer.
How to Access Bulk-Billed Surgery?
To access bulk-billed cataract surgery, patients need a referral from their general practitioner (GP) or optometrist. It’s important to research and contact local hospitals or clinics in Canberra that offer bulk-billed services.
Costs of Private Cataract Surgery
For those who prefer private treatment, understanding the costs involved in cataract surgery is crucial. Private surgeries often offer quicker access to treatment and a broader choice of surgeons.
Private Cataract Surgery Prices
Private cataract surgery prices can vary significantly based on several factors, including the surgeon’s fees, hospital charges, and the type of lens used. On average, the cost of private cataract surgery in Australia ranges from $3,000 to $5,000 per eye.
Factors Influencing the Cost
Surgeon’s Fees: Experienced surgeons may charge higher fees for their expertise.
Hospital Charges: Different hospitals have varying charges for operating room use and other facilities.
Lens Type: Premium lenses, such as multifocal or toric lenses, can increase the overall cost.
Health Insurance and Out-of-Pocket Expenses
Private health insurance can cover a portion of the cataract surgery costs, depending on the policy. However, patients should be aware of potential out-of-pocket expenses, which can include:
- Surgeon’s gap fees
- Anesthetic fees
- Additional tests and consultations
Comparing Costs in Different Regions
The cost of cataract surgery can also vary based on location. For instance, cataract surgery costs in Brisbane might differ from those in Sydney or Melbourne. It’s advisable to get quotes from multiple providers to compare prices and services.
Cost of Cataract Surgery in Canberra
Cataract surgery costs can vary widely depending on several factors. In Canberra, the price typically includes pre-surgery consultations, the procedure itself, and post-surgery follow-ups.

Factors Affecting Cost
Type of Surgery: Standard cataract surgery might differ in cost from surgeries that use advanced technology lenses.
Surgeon’s Experience: More experienced surgeons may charge higher fees for their expertise.
Hospital Fees: Costs can vary depending on whether the procedure is performed in a public or private hospital.
Insurance Coverage: Your out-of-pocket expense will depend on your health insurance policy and whether the surgery is performed in a hospital covered by your plan.
Average Cost
In general, cataract surgery in Canberra can range from $3,000 to $4,000 per eye or more. This can vary depending on the factors mentioned above.
It is important to consult with a few different clinics to understand the full scope of what each offer and how it affects the cost. Ensure you discuss all possible expenses with your surgeon before proceeding.
In Canberra, the cost of cataract surgery may vary between public and private hospitals. Medicare coverage is available for public procedures, while private surgeries require additional considerations of insurance and out-of-pocket costs.
Cataract Surgery for Pensioners
Pensioners in Australia have specific considerations when it comes to cataract surgery costs. They often have access to additional concessions and benefits.
Pension Concessions
Pensioners may receive reduced fees for cataract surgery through public health services. It’s essential for pensioners to check with their healthcare providers and Medicare for available concessions.
Conclusion
Understanding the eligibility for free cataract surgery and the costs involved in private surgeries is crucial for making informed decisions. Whether opting for Medicare-covered procedures or choosing private treatment, patients should thoroughly research their options and consult with healthcare providers to ensure the best care possible.
At Junic Eyecare we understand how to navigate the referral systems for our patients. Make an appointment to see one of our optometrists by calling 02 6152 8585 or booking online on www.juniceyecare.com.au.

CANBERRA OPTOMETRIST
Juliet obtained her Doctor of Optometry degree from the University of Benin, Nigeria in 2006. She completed an internship programme before migrating to Australia, where she completed a master’s degree in public health at the University of Sydney in 2014. Following this, Juliet obtained a Master of Orthoptics from the University of Technology Sydney (UTS) in 2017.
Juliet has completed her competency in optometry examination with OCANZ (Optometry Council of Australia and New Zealand), and obtained her ophthalmic prescribing rights from ACO (Australian College Of Optometry Victoria). Juliet has worked in various positions, including retail Optometry, the Ophthalmology Department at Canberra Hospital, and more recently, at the John Curtin School of Medical Research (ANU).
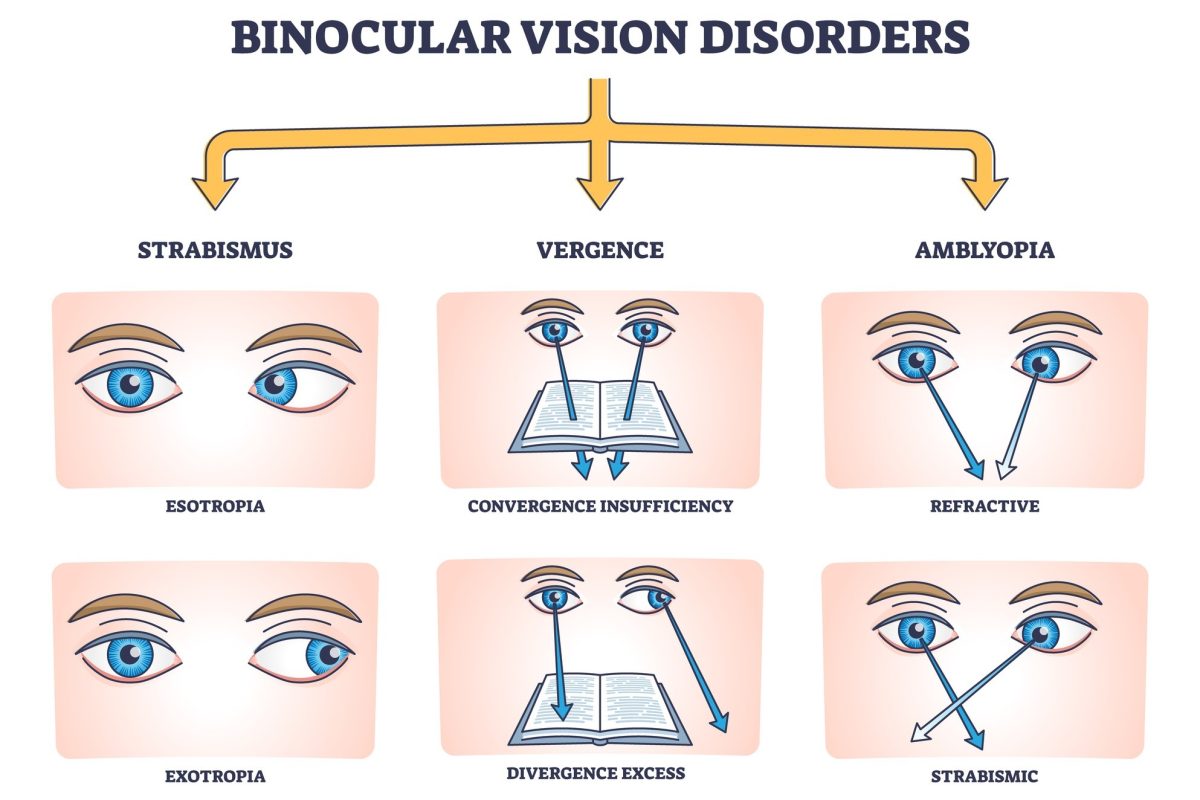
As a dedicated Canberra optometrist, Juliet is passionate about helping people with low vision, and binocular vision anomalies hence her interests in Low Vision Rehabilitation, Eccentric Viewing Training and Paediatric optometry.