Obstructive sleep apnoea (OSA) is a common sleep disorder characterized by repetitive episodes of partial or complete upper airway obstruction associated with hypoxemia and re-oxygenation sequences. OSA is more prevalent in men than women. It increases 2-3 times in persons more than 65 years old but sometimes can be seen in children with Adenotonsillar hypertrophy. The most important risk factor is a 10% weight gain which increases the risk of developing OSA by six times.
Sleep apnoea has various ophthalmic presentations which includes:
Floppy Eyelid Syndrome (FES):
This is a condition where the upper eyelid becomes elastic and easily folded upwards due to mechanical trauma to the eyelids during sleep. This is usually seen in association with papillary conjunctivitis, eyelid trauma and corneal epithelial erosions. Seen commonly in obese patients due to weak tarsus.

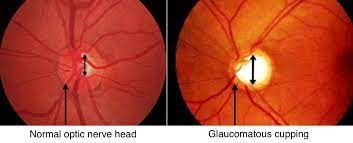
Glaucoma:
Glaucoma is an optic neuropathy or injury to the optic nerve which manifests as visual field defects. Glaucoma occurs in OSA patients because of vascular and mechanical factors. Vascular factors include periods of hypoxia followed by oxidative stress during reperfusion. Mechanical factors comprise increased IOP at night due to changes in sleep architecture and increased sympathetic tone.
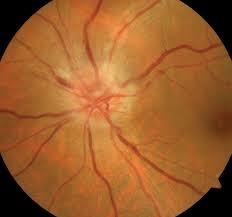
Nonarteritic Anterior Ischemic Optic Neuropathy (NAION):
NAION is a condition characterized by sudden and painless unilateral vision loss, oedema of the optic disk, and a relative afferent pupillary defect. Patients with OSA are more susceptible to developing NAION because of a combination of hypoxia, oxidative stress and increases intracranial pressure during their apnoeic episodes. Patients with OSA have 16% more probability to develop NAION compared to patients without OSA, and the prevalence of OSA in patients with NAION may be as high as 71%-89%.
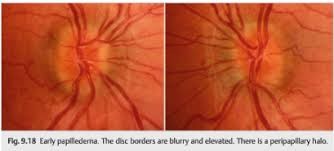
Papilledema:
Papilledema is a bilateral swelling of the optic disc. This condition when seen in OSA patients could be because of increase in their intracranial pressure during sleep occurring from hypoxemia during apnea episodes.
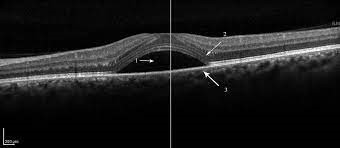
Keratoconus:
This is a bilateral condition characterized by progressive thinning of the cornea, irregular astigmatism and protrusion of the central cornea creating conical appearance. Its pathogenesis in patients with OSA is not well understood yet. But males with keratoconus with a family history of OSA is more likely to develop OSA.

Central Serous Chorioretinopathy (CSCR):
This is a serious detachment of the neurosensory retina at the macula. Approximately two-thirds of patients with CSCR have OSA. One theory for this increased prevalence is the presence of augmented oxidative stress, which can produce endothelial cell damage and vasoconstriction.
Why should I get an eye examination if I have sleep apnoea?
Patients with OSA bear an increased risk for several vision threatening ocular conditions. Optometrists as a primary eye care providers are optimally equipped to identify these ocular manifestations. At JUNIC EYECARE PLUS COOMBS we collaborate with ophthalmologists, your primary physician and sleep specialists to appropriately manage these conditions if they arise. These ocular conditions will require close monitoring to prevent permanent vision loss in OSA patients.
What are you waiting for? If you are in Canberra, get an eye checkup at Junic Eyecare Plus Coombs.
Phone: 02 6152 8585
REFERENCES:
- Wong, B., & Fraser, C. (2019). Obstructive Sleep Apnea in Neuro-Ophthalmology. Journal of Neuro-Ophthalmology, 39, 370-379.
- Huon, L.-K., Liu, S. Y.-C., Camacho, M., & Guilleminault, C. (2016). The association between ophthalmologic diseases and obstructive sleep apnea: a systematic review and meta-analysis. Sleep Breathing Physiology and Disorders, 1-10.
- Skorin, L., & Knutson, R. (2016). Ophthalmic Diseases in Patients with Obstructive Sleep Apnea. The Journal of the American Osteopathic Association, 116, 522-529.
- West, S. D., & Turnbull, C. (2016). Eye disorders associated with obstructive sleep apnoea. Curr Opin Pulm Med, 22, 595-601.

CANBERRA OPTOMETRIST
Juliet obtained her Doctor of Optometry degree from the University of Benin, Nigeria in 2006. She completed an internship programme before migrating to Australia, where she completed a master’s degree in public health at the University of Sydney in 2014. Following this, Juliet obtained a Master of Orthoptics from the University of Technology Sydney (UTS) in 2017.
Juliet has completed her competency in optometry examination with OCANZ (Optometry Council of Australia and New Zealand), and obtained her ophthalmic prescribing rights from ACO (Australian College Of Optometry Victoria). Juliet has worked in various positions, including retail Optometry, the Ophthalmology Department at Canberra Hospital, and more recently, at the John Curtin School of Medical Research (ANU).
As a dedicated Canberra optometrist, Juliet is passionate about helping people with low vision, and binocular vision anomalies hence her interests in Low Vision Rehabilitation, Eccentric Viewing Training and Paediatric optometry.

